Doctors have found a potential treatment.
A recent study has demonstrated that a novel antimicrobial compound can effectively combat “flesh-eating” bacterial infections in mice. This new compound might represent the beginning of an entirely new class of antibiotics, which researchers believe could be crucial in combating antibiotic-resistant bacteria.
Scott Hultgren, a co-senior researcher and professor of molecular microbiology at Washington University School of Medicine in St. Louis, highlighted the growing challenge of multi-drug-resistant bacterial infections. “Bacterial infections are a major health issue, and their resistance to multiple drugs is making them increasingly difficult to treat,” he noted.
The newly discovered class of antibiotics, named GmPcides (short for gram-positive-icide), is based on a molecule known as ring-fused-2-pyridone. GmPcides specifically target gram-positive bacteria, which are responsible for severe infections such as drug-resistant staph infections and toxic shock syndrome.
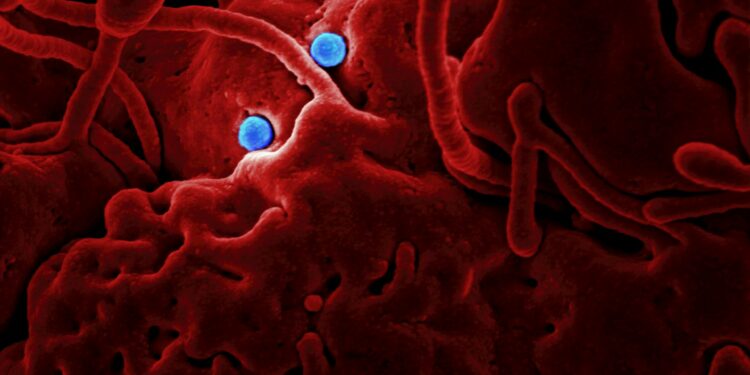
These gram-positive bacteria are known for their thick cell walls and their ability to release harmful toxins during infections. Michael Caparon, another co-senior researcher and professor of molecular microbiology at Washington University, stated, “All the gram-positive bacteria we tested have shown susceptibility to this compound, including enterococci, staphylococci, streptococci, and C. difficile, which are significant pathogenic bacteria.”
In their study, researchers concentrated on Streptococcus pyogenes, which is responsible for approximately 500,000 global deaths annually, including cases of flesh-eating disease. Mice treated with GmPcides showed better outcomes compared to untreated mice: they experienced less weight loss, had smaller ulcers, and exhibited faster recovery from the infection.
GmPcides were found to reduce bacterial damage and accelerate skin healing in infected mice. However, the precise mechanism behind the effectiveness of GmPcides remains unclear. The compounds appear to disrupt bacterial cell membranes, making them more permeable and thus impairing the bacteria’s ability to spread and cause harm.
Caparon explained that GmPcides alter the cell membranes of bacteria within minutes of treatment, leading to increased permeability and potential damage. This disruption is believed to be a key factor in the compound’s effectiveness.
Additionally, GmPcides seem less likely to induce drug-resistant bacterial strains. Preliminary experiments suggest that very few bacteria can survive exposure to GmPcides and develop resistance.
The discovery of GmPcides emerged unexpectedly during research aimed at preventing bacterial adhesion to urethral catheters, a common cause of hospital-associated urinary tract infections. The researchers were pleasantly surprised to find that GmPcides could effectively combat a range of bacterial strains in laboratory tests.
Despite these promising results, significant research remains before GmPcides can be made available in hospitals and pharmacies. The compounds must undergo further animal studies and human clinical trials before they can be approved by the U.S. Food and Drug Administration.
































Discussion about this post