The culprit has been found.
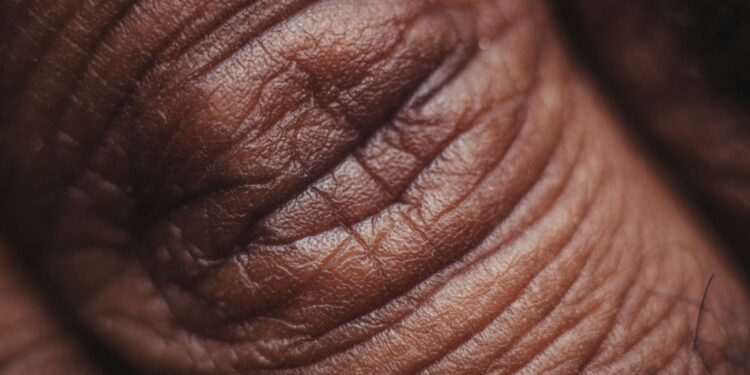
A recent study suggests a potential connection between consuming ultraprocessed foods and psoriasis, a chronic autoimmune skin condition. Conducted by Dr. Emilie Sbidian and her team at Henri-Mondor Hospital in Créteil, France, the research examined the dietary patterns of over 18,500 participants. The analysis revealed that individuals with active psoriasis were more likely to consume higher amounts of ultraprocessed foods. The study, published in JAMA Dermatology, adds to the growing evidence of the adverse health effects associated with these heavily processed products.
Ultraprocessed foods are highly modified products made from ingredients like refined starches, sugars, and unhealthy fats, often combined with artificial additives to improve flavor, texture, and shelf life. Common examples include sugary cereals, packaged baked goods, frozen ready-to-eat meals, and processed meats. These foods have already been linked to chronic health conditions, such as cardiovascular disease, type 2 diabetes, and inflammatory bowel disease.
The study found that individuals with active psoriasis had a 36% higher likelihood of falling into the top tier of ultraprocessed food consumption compared to those without the condition. This association persisted even after adjusting for variables like age, alcohol use, body mass index, and other health conditions. These findings suggest the connection between ultraprocessed food intake and psoriasis goes beyond the effects of obesity alone.
Although the research identified a strong correlation, it did not establish a direct cause-and-effect relationship. The findings emphasize the need for further investigation into how diet, particularly ultraprocessed food consumption, impacts autoimmune and inflammatory diseases like psoriasis. This research also highlights the broader risks associated with ultraprocessed foods, encouraging healthier dietary choices as part of managing and potentially preventing chronic health issues.
































Discussion about this post